“Sometimes what appears to be a catastrophe, over time becomes a strong foundation from which to live a good life.”
~ Dr. Rachel Naomi Remen
We Are All Unique
A year ago, I shared my decision to start medication after 4 years on the paleo autoimmune protocol (AIP). Almost one month after my original post went live, I started receiving questions from readers, wanting on update on my medication journey. Why did it take me a year to write this update on my results? Because the immune system doesn’t regulate quickly. Medication is a slow experiment that takes time. While some people have immediate and magical response to the first autoimmune medication they try, that’s pretty rare. I spent the past year tuning into my body, making conscious choices about which medications to try (and when), and carefully measuring benefits vs. side effects until I found something that works well for me.
Some of you asked for an update because you cared about me and hoped I was doing well. I appreciate that more than words can express. You were all incredibly kind and supportive when I announced my decision. Some of you are following my journey closely, because you are in the process of making medication decisions yourselves. Believe me, I empathize with that struggle. A word of caution, though: there is no one medication that’s right for everyone. If there was, a rheumatologist’s job would be much easier. The truth is that we each respond to medication differently. Just like the paleo autoimmune protocol, medication is a grand self-experiment where we each learn what does and doesn’t work for us. I share my journey on this blog to connect with people on a similar path and help us all feel less alone. But please don’t take my experience as a blueprint for your own. This is my unique experience, not medical advice.
My Medication Experiment
- Baseline: When I originally went on the AIP, within 1 year my symptoms had reduced by 95% and my flares went away altogether. I stayed stable at that level for 2 years. Then, the hormone shifts that precede menopause caused an increase in rheumatoid arthritis symptoms again. While they never reached the extreme pain of RA onset, they brought a new symptom: joint changes. Those can quickly become permanent with rheumatoid arthritis, which is why I decided to try medication. (You can read the details of my struggle with that decision here.) The symptoms I was experiencing pre-medication were: (1) significantly reduced range-of-motion in my left shoulder, (2) inability to make a fist with my hands, (3) foot soreness that limited my walks to 1 mile, (4) “mini flares” happening throughout the joints in my body, bringing extra inflammation to a joint for a few days or a few weeks at a time, and (5) I needed 1 Aleve twice daily for pain management (something that had always been true during my 4 years on the AIP.)
- Methotrexate: My rheumatologist wanted me to take methotrexate, prednisone and Humira all at once. That’s a standard protocol for someone with severe rheumatoid arthritis (which I have). I wasn’t comfortable doing that, because I wanted to be able to feel what each medication did for my body – positive and negative. So, with my doctor’s knowledge, I started with methotrexate alone. I began with a small oral dose (10 mg), and when that was ineffective I was slowly tapered up, eventually reaching the maximum dose of 25 mg. I was also switched from oral to injectable for maximum absorption. Results? It improved my lab inflammation markers (CRP and ESR) but had no impact on my joint inflammation itself. My doctor said this was frustratingly common. I took 800 mcg methylfolate to help mitigate the side effects. While that did help, I still experienced some hair loss, fatigue, and intermittent nausea. I tried increasing the methylfolate dose, but it made me anxious and didn’t improve my side effects further. The side effects weren’t debilitating, however. If the methotrexate had been effective, I could have managed. I stayed on methotrexate during my other medication trials, since it can sometimes make other medications more effective. However, once I found a biologic that worked (see below), I stopped the methotrexate with no negative consequences. This classifies me as a “non-responder” to this medication.
- Prednisone: Next, I tried a prednisone taper on top of the methotrexate. My doctor hoped this would dramatically reduce my inflammation while giving the immunosuppressant time to work. This was my first experience with steroids. I had always thought prednisone was stronger than over-the-counter NSAIDs. In fact, when I started prednisone, my doctor told me to stop taking Aleve for two reasons: (1) It should no longer be necessary, and (2) combined with steroids there’s an increased risk for ulcers. However, my pain spiked when I switched from Aleve to prednisone, even at the peak of the taper: 30 mg. I also experience many negative side effects: mood swings, extreme thirst, blood sugar imbalances, less ability to manage stress, fluid retention, bruising bodywide, dark circles under my eyes, and eventually collapsing veins making blood draws difficult. Following my doctor’s recommendation, I gave this a 3-month trial, but was very happy to get off this medication. Because I experienced so little benefit, it was easy for me to taper. Prednisone can be addictive for a lot of people; I’m grateful that wasn’t true for me. So, that’s two medications that didn’t work for me.
- Cortisone Shot: These are injectable steroids focused on a specific joint where inflammation is high. The biggest motivation for my trying medication was active joint damage happening to my left shoulder. I was experiencing major loss in range-of-motion and increasing pain. Since neither the methotrexate nor the oral prednisone had any impact, the doctor agreed to try a cortisone shot. The shot dramatically improved the pain, but unfortunately didn’t improve the range-of-motion.
- Humira: At this point, it was time to try a biologic. My doctor recommended Humira or Enbrel. My insurance approved Humira, so that’s the one we tried. This was my first improvement in RA symptoms after months of medication experiments. I regained my ability to make a fist, and inflammation elsewhere in my body lessened. I was less stiff/guarded, and people in my life noticed I moved more quickly and easily. These improvements happened within the first 2 months of taking the medication, but I wasn’t in remission. I still had some inflammation in my hands, wrists, shoulder, and feet. My doctor said it can take 6 months to see maximum benefit, so we waited but I had no further improvements. In fact, I ended up having the largest flare I experienced since going paleo. This was somewhat of a shock, because I had hoped medication would prevent flares from happening, and this proved untrue. When it comes to RA medication, results are mixed. In terms of side effects, Humira seemed to make my methotrexate side effects worse: I felt increased nausea and fatigue on the weeks when I took both. I switched to taking my injections right before bed, so I could sleep off some of the side effects.
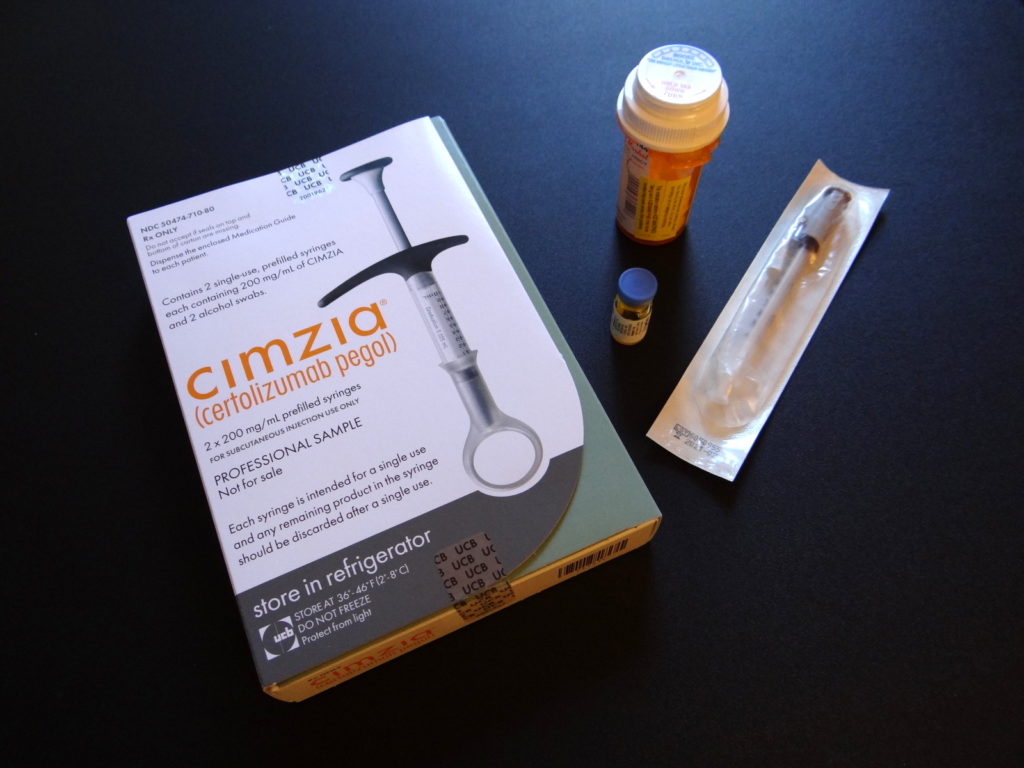
- Cimzia: At this point, I started to lose hope that any medication would help me reach remission. But I switched to a new doctor, who suggested Cimzia: another biologic in the same category as Humira (TNF inhibitor), but Cimzia is formulated differently. My doctor said that Humira is released immediately and dispersed throughout the body equally, whereas Cimzia circulates through the body in a protective coating and is designed to release in areas of high autoimmune activity. He hoped it would be more effective at reaching the inflammation that remained, and it was. Within a few months, almost all of my inflammation disappeared (including the lingering flare). It’s the closest I have ever felt to remission. I was able to stop the methotrexate and the Aleve altogether. I had already stopped the prednisone, so Cimzia is now a solo medication for me. I experience no side effects now, and I’m glad that I didn’t give up when the first medications I tried failed.
Remission?
Why do I have a question mark after that word? Because remission has a fluid definition which means different things to different people, and the medical definition continues to change as well. This is what it means to me right now. This is the best I have ever felt in 5 years with RA.
- I no longer need any painkillers at all.
- I have also reduced my supplements.
- I have no morning stiffness.
- I move more freely throughout the day and evening – no guarding of my joints.
- My joints are stronger bodywide.
- I’m capable of a wider range of physical activities.
- I sleep more comfortably.
- Fatigue is a very rare feeling.
- There is no sign of active joint damage.
However, it’s not perfection. While most days I am symptom-free, with no tender joints at all, I occasionally feel a pulsing in a joint or an increase of inflammation for a day or two. These are usually hormone-driven, just as they were prior to going on medication. The difference now is that there is no loss in range-of-motion. My doctor doesn’t classify these as flares because they are mild, pass quickly and cause no damage.
I don’t give medication all the credit. My healing diet and lifestyle work together with my medication to achieve these results. And while I have stopping many supplements that are no longer needed, I still take a few that I find beneficial: curcumin, boswellia, and krill oil. This combination makes up my personal RA treatment protocol.
Medication Isn’t Always a Villain
I was terrified of going on medication, and I know many of you have the same fears. Leaders in the real food and natural health communities repeatedly warn about the dangers of medication, especially immunosuppressants. But here’s my question: why aren’t they also knowledgeable about the benefits? Why is it presented as an “either/or” choice? While it’s true that medication can sometimes cause more harm than good, with careful monitoring and trial and error, we can often find a medication that offers great benefit. An active autoimmune disease can become disabling and even life-threatening. While diet and lifestyle can definitely help minimize our symptoms, it’s not a cure. The same goes for functional medicine – it can remove obstacles to healing but doesn’t remove autoimmune disease altogether. The practitioners I admire the most make room in their treatment plan for both conventional and alternative approaches. This doesn’t mean I think everyone should be taking medication. Rather, I think we need to remove the stigma associated with this choice. The goal is to live the best life possible with autoimmune disease. Why deny ourselves any tools in the toolbox? We always hear about negative medication side effects, but I’ve experienced beneficial ones. In addition to reaching remission:
- I no longer have adrenal fatigue. I was experiencing hormone fluctuations and adrenal fatigue prior to going on medication, and no amount of adrenal support – either through lifestyle or supplements seemed to make a difference. Cimzia ended up having the biggest positive impact on this problem, because it turned out that rheumatoid arthritis activity was the root cause of my adrenal fatigue.
- I tolerate more foods now. I think the reason for this is two-fold. One is that medication has reduced my immune system’s “army”, so there are less soldiers to attack when I encounter an inflammation trigger. The second reason is that medication actually improved my gut health. How? Leaky gut is a trigger for autoimmune disease, but it’s also a side effect of having autoimmune disease. No matter what our diagnosis, the immune system also attacks the gut. This means it’s very difficult to heal leaky gut unless we are in complete remission. When intestinal permeability remains, we are more prone to food intolerances due to the food chemicals slipping through to our bloodstream in larger molecules than our body can use. This can set off an inflammatory response. Some foods that used to cause autoimmune flares in the past for me (like dairy and nightshades) no longer seem to do so. This doesn’t mean I’m bingeing on these foods, but in the past, trace exposure would have set off a flare. Now, I can eat them occasionally.
- My immune system still works. Alternative health practitioners will often say that these drugs turn the immune system off. If that were true, we wouldn’t be able to leave a sterile environment, and every day would be life-threatening. The goal of immunosuppressants is to suppress an overactive immune system down to a healthy level. Sometimes this is a balancing act, and people end up with more illnesses as a result. That didn’t happen for me. I caught one cold which healed completely within a few weeks. There was no advanced infection. That has been my only illness.
- My labwork is excellent. Before going on medication, my white blood cells showed unusual activity (no surprise with autoimmune disease). Cimzia moved them into optimal health ranges. My inflammatory markers (CRP and ESR) dropped to normal. And while I get bloodwork regularly to monitor liver and kidney function (which is important when taking immunosuppressant medication), my tests show healthy function of both.
- I currently experience no negative side effects. When we read the list of potential side effects of these medications, it’s no wonder we feel frightened. We picture getting all of them, but it’s important to realize that they don’t happen to everyone. The goal is to find a medication we tolerate well. Cimzia is currently offering me great benefit with no drawbacks. If you look at my medication experiments, you will see that I tried and discarded other medications when the opposite was true. Just because one medication fails to help, doesn’t mean they all will.
Shoulder Replacement Surgery
Yet, medication’s not a miracle. As I’ve mentioned above, one of my primary motivations for trying medication was a rapid loss in range-of-motion in my left shoulder. My hope was that I could halt and reverse this process. Unfortunately, that didn’t happen. My body’s variation of rheumatoid arthritis moves rapidly when it’s active. Damage happened before I even got in to see the doctor, and continued happening until we tried Cimzia 10 months later. In my podcast with rheumatologist Dr. Melissa McNamara, she said it is possible to reverse very small erosions, but once they reach a certain size, she’s never seen them reverse.
When the nurse called with the results of my x-rays she told me there was severe damage to the joint, and the doctor recommended an immediate surgical consult. I was devastated, and I didn’t accept it at first. I tried physical therapy, acupuncture, and a number of different types of bodywork. While I would temporarily get a little range-of-motion back, it was minimal, and the results didn’t last. This is why: I had zero cartilage remaining in my shoulder, severe erosion to the bones, and a re-shaped joint that acted as a third physical barrier. I finally made peace with reality and followed through on joint replacement surgery this year. It was an emotional journey to get there. Right now, I feel grateful for a skilled surgeon, excellent insurance, and a wonderful physical therapist. I had no surgery complications and recovered well. I’m currently rebuilding my shoulder strength and function and making gains every week.
So, the question is: could I have avoided this if I had gone on medication sooner, instead of delaying 4 years? This is one of those “what if” questions that can never truly be answered. It’s the path not taken, and there are so many variables. The answer is: maybe yes, maybe no. Many people experience joint damage even when taking medication. I’m not the first RA patient to have joint replacement surgery. At RA onset, my body was cripplingly inflamed, malnourished, and pretty toxic from years of eating processed foods. All of this is guesswork, but I think medication would have been very hard for me to tolerate and I’d have suffered more side effects back then. I also don’t think I would have tried diet simultaneously, so the excruciating pain I was experiencing would likely have continued for many months before finding relief, if ever. I think I would have felt victimized instead of empowered.
I don’t regret the choices I made before now. I made the best choice I could at each stage of my journey. But I want to be honest about everything, including this.
If You Still Need Medication, What’s the Point of Paleo?
When I first started my medication trials, I hoped that I would respond well to the mildest medication, since I had already reduced so much of my inflammation naturally. This obviously proved untrue for me. While I was disappointed, I was also more grateful than ever for the paleo autoimmune protocol. It took me almost a year to find a medication that helped. Dietary intervention started helping within just a few weeks and continues to help me to this day. If I was still driving inflammation with poor diet and lifestyle choices, I don’t know that I would ever have found a medication that worked. I also believe that my non-toxic diet and lifestyle make it easier for my body to process and tolerate the medication.
I’ve seen 3 rheumatologists in the past year. The first one said that diet indeed has strong pain-relieving effects for patients. The second one said that my diet and lifestyle clearly managed my pain and slowed down my disease process as well; it simply wasn’t able to stop it altogether. My current doctor and I don’t talk about diet at all, but he is stunned by my health. It’s not what he usually sees among his patients. Normally, people with RA take multiple medications and still need painkillers anyway. His advice? “Keep doing whatever you’re doing.”
It doesn’t have to be either/or. For me, I see diet and lifestyle as complementary medicine. This combination is what feels most supportive of my health. I also asked this question to a number of my peers; here are their answers.
What’s Next For Me?
- My goal is to continue to live the best life possible with autoimmune disease.
- I have no desire to go off my medication at this point. It’s offering benefit without harm, and I don’t want to risk more permanent joint damage.
- I’ve been experimenting with food reintroductions. I still plan to stay paleo with a focus on nutrient-density, but if I could expand my range of options simply for the occasional restaurant convenience, I would love to do so. I don’t plan to attempt reintroducing gluten. The risk is simply not worth it to me. I believe what Terry Wahls says: “What we eat and how we live sends a direct message to our bodies about how to respond: with vitality, or with decline.” I plan to support my body for continued good health.
- A peaceful, positive mindset. Sustained remission is rare with rheumatoid arthritis. I can’t count on always feeling this good. However, I don’t live in fear of this. I live in gratitude. My goal is to enjoy my good health each and every day, and I hope my remission lasts. But if it doesn’t, I will nurture myself with self-love and grace (because flares aren’t permanent either).
My Advice For You
- Medication is a very personal decision. I can’t tell you what to do when facing this choice. But if you are not in complete remission of your autoimmune disease, and damage is happening to your body right now, medication has the potential to help and I believe it’s worth considering.
- If you choose to take medication, expect it to be an experiment with some trial and error. Just because one medication fails, doesn’t mean they all will. That’s where the statistics can be misleading. When you hear that only 1 in 4, or 1 in 7 people respond to a medication, that doesn’t mean medication doesn’t work for most people. It means you may have to try many different ones before finding the one that helps your unique body.
- Keep a symptom journal. Since medication trials take time, it’s easy to forget where we started, notice all the improvements, and track side effects accurately. Keep notes, so you can more clearly see what is and isn’t working as you go along. If I hadn’t done so, I wouldn’t have been able to make effective medication decisions myself, and this blog post wouldn’t be filled with the details I’ve been able to share with you.
- Find a doctor you trust to guide you through this experiment. Make sure it’s a doctor who listens to you. Resources: Building Effective Doctor-Patient Relationships and Do Paleo-Friendly Autoimmune Specialist MDs Exist?
- The goal of medication is for the benefit to outweigh any negative effects. So, if you’re experiencing a high number of side effects with one medication, ask your doctor to recommend a different one instead. If your doctor tells you it’s normal for people with autoimmune disease to suffer, seek out another doctor. We deserve to feel good.
A Special Request
Since going public about my choice to take medication, I receive emails and suggestions from people who believe there is a “cure” I have not tried. While these might come from a true desire to help, I ask you to trust that in 5 years, I have tried a wide range of interventions and worked with many qualified practitioners. If you follow my blog and podcast, you know that I am knowledgeable about everything from functional medicine to energy medicine to allopathic medicine. There is very little I haven’t tried. I’m not looking for a new practitioner nor treatment suggestions at this time.
Disclaimer
This website has a disclaimer on its legal page that is always in effect, but since I’m talking about medication here, it seems prudent to end the article with this reminder: I’m neither a doctor nor a dietitian. This blog is designed to chronicle my own health journey, share what I learn in the process, and connect with others on a similar path. Everything I write here is simply my opinion and not a replacement for medical advice. Always consult with your doctor when making medical decisions.
My Journey







I am new to your podcasts and aticles (started just a few months ago). I have yet to hear you speak of IVIG. What are your thoughts on IVIG. I am currently praticing the AIP, but I am still having symptoms. I have SFN.
Hi Sue. I have no experience with IVIG, so I can’t offer an opinion.
I just love your heart, keep rising above it all. We CAN do this, graceful and true. Tender hugs , Ro
Yes we can indeed. Tender hugs to you as well.
Thanks for your post Eileen. I was diagnosed with RA 8 years ago at the age of 60 and chose not to go on medication. I went on the AIP diet 4 years ago which helped a lot with pain and flexibility. I do have damage to some of my joints especially on the joint of my middle finger on my right hand. I cannot bend the finger but all the others, I have morning stiffness which goes away during the day but back next morning. It’s like “Groundhog Day”, every morning the same story over again. My husband and I went hiking last September on the camino portugues from Porto to Santiago de Compostella. I hiked 200 km with a heavy backpack until my achilles tendons acted up. I could eat any food without having flares but as soon as I came back to Canada and started eating the food here I started to have pain. I’m back on strict AIP for a while til things calm down and then reintroduce some foods I would like to eat again. I don’t know if I did the right thing by not going on medication but I just couldn’t do it. I do consult with a naturopath.
Connie, there is no right and wrong decision. We each need to do what’s right for us, and there’s a wide spectrum of severity when it comes to autoimmune disease. It sounds yours is mild, which is wonderful. That trip sounds amazing! May you continue to live a full and beautiful life.
Thank you so much for posting this. Im sever stage 3 hidradinitus supparativa and have been AIP for 2 years. I didnt know at the time that Aip was only a temp thing and have lost oral tolerance to almost everything. Although i have improved a lot i am still unable to work and have been considering humira. I’m convinced that need it. I’ve already done all the other meds for years and if this one can help me regain oral tolerance than maybe i can establish a healthy gut again with legumes and more prebiotic foods
Hi Christopher. I’m so glad this post resonated with you. Thank you for writing. It’s actually a misconception that the AIP causes loss of oral tolerance. Rather, autoimmune activity and its negative impact on the gut can cause that (the same things that make people seek the AIP to begin with). That’s why it’s easy to mistake correlation for cause. However, you’re right that food tolerance often expands greatly during remission, and medication can sometimes help achieve that. I hope that’s true for you. There’s also a podcast you might find helpful, where we talk about functional medicine approaches to escalating food sensitivities. It’s Episode 93: Are You Eating Enough to Heal? Wishing you remission and an expanded diet soon.
Thank you so much for sharing your personal story Eileen and for this update. I have been following along with your journey for years now, since I was diagnosed with RA in 2017 at age 42. Our paths our very similar where for the first 2 years I have done everything possible, or so it seems. I’m having some new pain and a flare at the moment and some new joints are changing. And while this makes me incredibly sad, I am encouraged when I read your story. I’m seriously considering medication to stop the progression of the joint damage but really scared about potential side effects. Thank you for all you do for this community!
Hi Jenny. I understand that crossroads so well. I can tell you now that going on medication was one of the best decisions I ever made. I’m very grateful. Wishing you wellness, whatever you decide.
Wow! So glad I found your articles! I was diagnosed with RA about 4 1/2 years ago and have tried so many natural remedies which did seem to help. Went off birth control last February and the pain kicked in. Had all my hormone levels checked and they are fine so nothing to “fix” there. I have decided to go back to the rheumatologist and discuss meds. It was a hard decision but almost a relief at the same time. Hopefully it won’t take me too much experimentation to find the right thing. Thanks so much for sharing your encouraging story. I hope I have a similar outcome!
Hi Lisa. I know that feeling so well – the difficulty of the decision but also the relief that comes from making it. For me, it was one of the best decisions I’ve ever made. It’s now 2 years since I wrote this blog post, and I continue to feel great and grateful. I hope you have a similar outcome! Wishing you wellness in every way.
Thank you SO much Eileen for sharing and for the details. My journey has crossed so many of the same paths. I believe I am ready to go back to my rheumatologist which is a humbling step for me. I have the AIP protocol well in place and have tried LDI AND LDN among other things. My story is long as well, I will spare you but you have given me courage to check into Cimzia since I also can’t tolerate the Methotrexate.
I hope to get my life back soon. RA is a bugger.
Teri, I know this crossroads you are facing so well. I can tell you that now years later, I am so grateful I made the choice to add medication & the AIP together. Remission is a wonderful thing. I hope you find the medication that works best for your body. Sending love and support your way.
Very good reading. Thank you for posting. I have been doing AIP for 5 months now and have been on mtx. for 3 months and 2.5 mg. of pred. Simponi did not work for me so had first infusion of actemra 3 weeks ago. Like flipping a switch I woke up and no swelling or tightness in wrist or hands, and haven’t had any for 2 weeks. I still don’t have all my energy back and was just wondering how long it took for you to notice the increase in energy after your symptoms subsided? Can’t wait to see my Dr. in 2 weeks. Hoping to start tapering some of the other drugs. Best of luck to you.
Hi Steph. I’m so glad Actemra seems to be a good fit for you. Fatigue has so many potential factors. If your inflammation is just now starting to reduce, it makes sense that it might take more time for your energy to come back. I also experienced iron deficiency which is common with RA, so iron supplementation was one of my puzzle pieces. Blood sugar balance is key for me as well. You can ask your doctor about both of those things. I also have a podcast on the topic of troubleshooting Fatigue: Episode 119.
Thank you for sharing. As a former pharmacist I do see the value in a balance between what can be achieved through good diet and lifestyle… and then if (or when needed) still utilizing medication. Unfortunately medication is definitely not perfect and I am glad you had a helpful Dr who allowed you to trial one at a time so you could truly see what was helpful and what was not. It is really inspiring for you to share your knowledge and real life experiences with us. I hope the surgery goes/went well and assists with mobility etc.
Hi Vanessa. Thanks so much for writing. I’m doing very well. I’ve now been in remission for 2 years and am so grateful. As for my surgery, my doctor was excellent. I didn’t regain 100% range-of-motion in that shoulder, but he never promised me that. He said the surgery would eliminate my pain, and it did. That has allowed me to regain both function and strength, and it’s expanded my life in many ways. It’s funny how many movements I had adapted without realizing it. I’ve also been able to return to both yoga and strength training – 2 activities I couldn’t do prior to the surgery.
Eileen, thank you so very much for writing this and for sharing your experience and extensive knowledge. I have really enjoyed listening to your podcast as well, particularly the one with Dr. McNamara.
It’s wonderful that you’ve discovered a successful treatment method for yourself, and I really appreciate you sharing your experiences. Although I have not introduced medication into my protocol, it’s something that I may need to consider in future, and this all greatly helps in making that decision easier.
I was diagnosed with RA almost 3 years ago and have been following the Plant Paradox diet for nearly 2 years now, without any marked improvement. However, I do have leaky gut and have also had type 1 diabetes for nearly 25 years, and I realize that this impacts my ability to heal.
As such, I intend to carry-on with my diet and vitamin/supplement protocol for now, and hope to regain good health once again. However, if the time should come that I need to consider medication, your story has made me feel much better about the potential of doing so.
I have just one question for you – as the costs of supplementation/medication and treatment of autoimmune disease is significant, and likely life-long, I’m wondering if you would be willing to share the name of your excellent insurance provider? They can certainly be hard to find!
Thank you once again,
Susan
Hi Susan. I’m very lucky that the Affordable Care Act was signed into law before I went on biologic medication. You’re right that the cost is very high. I get my insurance through Healthcare.gov. My premiums aren’t cheap, but it’s a fraction of the cost of my medication.
Eileen, such a great post. I’m so very happy for you. I have been on a couple biological that had side effects and just got approval from my insurance for Cimzia. I am expecting great results. Thank you for your honest and vulnerable thoughts on this process. It’s a tough road but there is much hope and many who encourage us along the way. I’m very grateful for you♥️
Kathy, you’re so welcome. I hope Cimzia is a great healing partner for you as well!
Hi Eileen. I recall when you bravely shared your decision to take medication on the blog a couple years ago, and had been wondering how that had gone for you. I’m a little late on finally seeing this post, but I’m happy that you found the right combination of treatment options for you and are doing well with them. Thanks for all that you do for the AIP community!
Hi Eileen! I really appreciate you sharing your journey with all of us. I was diagnosed in November 2017 and my doctor said with my labs it’s usually aggressive. I had only been on one medicine for my thyroid since 2015. I have spent hours researching and trying not to take meds. Right now I’m on plaquenil and I feel like it’s doing nothing. Also the pain in getting worse (unbearable in my wrists and hands). Like you, I use my hands for work, doing facials. I know I need more meds. I take meloxicam for pain and it does nothing. Being a non drug user my whole life, I’ve decided to check into medical marijuana. I was curious your take on that or did you find other things to help with pain. Pain killers scare me as I know people that are addicted to them. Thank you, Toni
Hi Toni. Since I’m not a doctor, I can’t advise you, but I can share what I’ve learned as a member of this community. Some people find medical marijuana to be a very effective pain reliever, but my understanding is that it doesn’t prevent joint damage. So while it might worth trying as a potential substitute for meloxicam, it wouldn’t necessarily replace your need for a stronger immunosuppressant. That said, pain management is essential to quality of life, so it’s definitely worth a try! Two podcasts that might interest you are: Episode 49: Rheumatoid Arthritis with Dr. Melissa McNamara and Episode 33: Medical Marijuana and Autoimmune Disease. Wishing you wellness in every way.
Thank you so much for your response and information on the podcasts. I definitely understand I will need an immunosuppressant but was thinking about pain. It really helps to find people who are further along on this journey that can help inspire us and share their stories.
I am so impressed by your journey and the honesty of your success and failures. I too was hesitant to take medication for RA, but could not tolerate the pain. I was diagnosed in 2017 and started methotrexate shortly after. I saw a new doctor and she switched me to Remicade infusions every 8 weeks. Plus 5 mg of mtx. Fortunately I did not have any joint damage. My esr and Crp have reduced to a normal range. Now I am dealing with osteoarthritis. I am recovering from total hip replacement . (Age 67)
Like you, I have been active throughout my life, healthy diet. A month before my symptoms started, my husband and I were hiking at Zion national park.
Bless you on your journey
Sue
Susan, thank you so much for sharing your story. That’s wonderful that you’ve had no joint damage. If you haven’t tried the paleo autoimmune protocol, I recommend it – not as a replacement for your medication, but as a complementary practice. It’s highly pain relieving for both osteoarthritis and RA joint pain. Wishing you a smooth surgery recovery, pain-free days & nights, and hikes in your future!
Thank you Eileen, I am hoping for better days ahead as well. I noticed years ago that I would get a burning sensation in my mouth when I ate certain foods, and my tongue would look “scalloped.” I have since learned that the tongue is a good indicator of health. I stopped gluten years ago as per my endocrinologist for hashimotos. This year I read about autoimmune protocol and eliminated nuts, and all dairy. I eat meat , and lots of fruit and vegetables. When I tried almonds after a few weeks I had the burning of my tongue again. I have been dairy sensitive for years and did not drink milk, but cheese was ok. Now I have eliminated that as well. Sugar also causes tongue symptoms for me. I have very little in the way of baked goods and processed foods.
You are a motivation! I have MS and deeply struggled with the decision to take medication. I have been on AIP very compliant for 2 years and have experienced some great benefits from this, but unfortunately not enough so to put my disease into remission. I too had to make the very difficult decision to start a disease modifying drug that I really did not want to have to take. However, I hope that the AIP diet will continue to help me achieve the excellent health I desire and like you, help my body tolerate this medication very well. Thank you for sharing your story.
You’re so welcome, Lindsay. I’ve learned that medication + the AIP can be a powerful combination. Wishing you medication success and remission in your near future.
I did AIP for the first time in January 2016, I thoroughly educated myself and strictly stuck to it for 8 solid months. I was 10 years into my RA journey and in very bad shape when I started. I decided to start AIP medication free and I think that was the kiss of death for someone so far along into the disease. But I got it into my head I was stupid and ignorant for putting poison into my body when diet alone could fix it all. Your book, Mickey Trescott’s one book, and The Healing Kitchen became my bibles. But in those 8 months, all that changed was losing 30 lbs. I was still in the worst shape of my life and my inflammation markers were at an all-time high. By August I was defeated and angry and while on our family vacation I fell off the AIP wagon, HARD. I went back to eating everything and I gained back those 30 lbs (and then some). I pretty much could be the poster model for the face of inflammation. My rheumatologist was as supportive as traditional doctors can and will be and he finally gave me an ultimatum, either he can help find me the least poisonous treatment and see what works or he can no longer treat me.
The year of 2017 will go down as the year I was a lab rat. I had already tried methotrexate before and not only did it do nothing for me, it made me a complete and utter zombie and I was not going to revisit that, so I went back on prednisone and Plaquenil. Nothing. He took me off Plaquenil and started me on sulfasalazine. Nothing. He prescribed me Arava. Nothing. It was time for biologics. I had taken Humira when I was initially diagnosed since I was disabled like you were at onset. Humira worked wonderfully, then I began to lose feeling in my toes and eventually my feet. They took me off it and it took three years to get the feeling back in my toes. So we tried Xeljanz, I liked it because it is the only biologic that isn’t an injection, but….it did nothing. I moved on to Orencia, it worked! I started to feel like myself again. Then my liver levels shot up. I had to go off it and during my time off it my health rapidly declined and once I went back on it never worked again. And now I am on Cimzia, and it is working. I was able to taper off prednisone successfully and I am taking nothing by Cimzia. Just this week I started to feel pain in my feet and one hip and this morning I woke up and my elbow hurts. Yesterday I got a terrible pain in my right ankle (not in the joint, in the tissue) and today my ankle is swollen, red, and warm to the touch (reminds me so much of onset). So I know my RA is trying to find a way around the meds and that is when I realized I need to get back on a healing diet because the combination of the two could be my key.
I remember reading your article about how you had to go back on medication and as sad as I was for you I found so much comfort in it. I selfishly resented reading how AIP took your RA from a scream to a whisper. Of course, I was happy for you but why wasn’t it doing the same for me? What was I doing wrong? It messed with me so much emotionally and mentally, I became extremely obsessive on AIP to the point that I felt like I had an eating disorder on top of my RA. Today I went hunting to find out if medication ever did work for you and if you were still on it. I was excited and surprised to read that Cimzia is also the treatment that is working best for you, this put a fire under me, even more, to get back on that AIP wagon. For some reason, this time feels harder than last time but I am going to do it, I have to do it. I work full time and have two kids, in the Spring my job did a 360 and has become quite stressful. Unfortunately, there is no escaping it so if I have to deal with stresses I can’t change I am going to have to change areas I have control of.
Thank you for always being the light for me. You don’t even know me, but you might be one of my biggest inspirations. Out of everyone in the AIP community you are my guru. Thank you!!!!
– Melissa
Melissa, what a journey you’ve been on! Thank you so much for sharing the details of your story. I do think diet, lifestyle, and medication can all be powerful partners in health. Let me share 2 podcasts that might really resonate with you: Trying to Do It All: Work, Family & Autoimmune Healing – Great tips from people in the same situation as you. And Self-Compassion with Dr. Kristen Neff – This podcast teaches a mind-body technique that really helps during difficult times, whether they are stressful times at work, or managing an RA flare. Sending lots of love your way. You’ve got this!
Eileen – I have to admit I have a big geeky girl crush on you even though I am more on the Keto side of the house – I think of paleo and keto as kissing cousins. I am not dogmatic about either as I feel there is often more than one pathway to health. I am still catching up on your podcasts, but I couldn’t find out if you have tried fasting in your healing journey? Particularly, extended fasting. My husband has psoriatic arthritis and suffered in constant pain with the standard of care. I am worried he is going to run out of biologics as he has built up immunities to several already. Of course keto and fasting is very synergistic, and I have done it and have researched it. He didn’t think he could manage learning/attempting a diet change, but could handle fasting. Even though he hasn’t been doing it that long, the benefits have been remarkable. Less pain, less meds, longer periods between treatments, enhanced range of motion yada yada. I won’t go on, as you may have tried it, and I know you are aware of practically every treatment protocol out there. Thanks for all you do.
Hi Carole. You are so sweet! I’m so glad your husband is finding fasting helpful. I have another reader with PsA who swears by fasting, too, although of course it’s not a long-term solution, because we do need to eat. My other reader does a multi-day fast under a doctor’s guidance a couple of times per year as an anti-inflammatory protocol. Like your husband, she finds it beneficial in combination with her medication. She also struggles to stick with a healing diet, so maybe fasting is especially helpful when the body is also being asked to process a lot of inflammatory foods? Fasting is intensely detoxifying – for some people it’s too intense, but for others it can be beneficial. For me, fasting seems to have the opposite effect – it increases my inflammation. I do naturally go 12-15 hours between dinner and breakfast, so my body gets a small break daily. But when I try to push further than that, there’s a net negative effect for me. One of the reasons I recommend the guidance of a doctor is to troubleshoot any negative effects and also guard against nutrient deficiencies. Some people who find fasting helpful can do it too long. Others will find fasting isn’t the right choice for them, and a daily healing diet is more beneficial.
Hi Eileen, thank you for sharing your story. I was diagnosed with RA in December 2010, a very stressful time in my life. i was immediately put on methotrexate which I took for only one month for fear of the side effects. In 2012 I quit my job, changed my diet, detoxed and did ozone therapy and in 2015 it seemed to have gone in remission. Went back into the working world, messed up my diet and it has been back every since to the point of some joint damage with my fingers. All this time only using Aleve. It has now gotten to a point where I had to seek medication which seems to be working. Maybe of I had continued using methotrexate i would not have any joint issues now, who knows. You mentioned something above about fear, fear of taking the medications because of the side effects and that is so true. I dare say that what we attract what we fear so let me say to all in this community, let’s put fear aside and do what we have to help our bodies heal. Tell ourselves each day that we are wholly and wonderfully made. Look in that mirror each day and say I love you. Once again Eileen, thank you for sharing your story as you continue to heal.
Beautifully said, Charmaine. Thanks for sharing your story and your wisdom.
I was diagnosed with RA 8 years ago… I could hardly wipe my own butt! I was pleased on 30 prednisone, plaquenel, enbrel and metheltrexate. I experienced very little relief. I was then diagnosed with sjogrens. About three years in I was diagnosed with celiac. Through aip, paleo and Primal I was able to get rid of some meds. I switched to Humira from enbrel… I still take methyltrexate. Recently I have experimented with very low carb…I am amazed as I am not even stiff in the morning! If you have RA you know how amazing this is. I am now experimenting with going longer between humira injections. I am beginning with moving from 14days to 20 days. My Dr. says there is evidence that one can reduce injections and stay in remission! I hope that will be true for me…but if not…I am ok with that. I am so grateful for modern medicine AND ancestral health! Thank you, Phoenix! Honestly, I have avoided your site for a couple of years because I felt guilty for being on meds. My Dr. says I had the highest readings he has ever seen for RA. It is not worth it to become disabled. Arthritis is the # 1 cause of disability in our country! I for one will do everything I can to preserve my health. I am now a certified Primal health coach through Mark‘s daily Apple. I have better health than I have ever had and I am 52! Thank you for your honesty. I hope you continue to heal.
Blessings,
Anna
Thanks so much for sharing your story, Anna. It was never my intention to alienate anyone who took medication. Even when I hadn’t yet made that choice, I never saw it as a failure for anyone else. Yet, I can see where you might have guessed otherwise. That’s one of the reasons I’m sharing my own journey so publicly. It’s true that the paleo community as a whole has demonized medication and celebrated medication-free success stories, above all others. Yet, many of us need the combination – not everyone – but there’s no shame in providing our bodies with the help they need. Like you said, it’s all about living our best life with all the tools at our disposal. I think it’s wonderful that you are now a certified Primal health coach. You will help many people with your holistic viewpoint and the empathy of personal experience.
Eileen, thank you so much for sharing your journey. I was diagnosed Sept 2016 with RA, quit my job as a hospice nurse and started AIP. My body responded well for about 10 months but then inflammation returned. After putting off my rheumatologist recommendation to start methotrexate, my FP MD pointed out that even at the age of 61 my body was in very good shape and why would I not want to try for a med that might help me. But I know that if I had not started AIP I wouldn’t be as healthy as I am now ( I was pre-diabetic and obese)! Your words show me that I made the right decision to start meds, though I agree one at a time. I seem to be responding well to methotrexate and only take Aleve about twice a week. So the journey continues. Thank you for all you do to educate and inform us.
Hi Carin. Thank you so much for sharing your experience. It sounds like you have a wise doctor. Diet + medication can be a powerful combination.
I’m so happy to know that you’re feeling well. I wish I could always hear this from other RA patients. I also have RA, since 2 years ago. On Feb 2016 I started avoiding gluten, dairy and processed foods when the doctor prescribed me methotrexate, but after 4 months I eat gluten and didn’t have any reaction. Same with dairy. I don’t know if I have any food intolerance. I take methotrexate + prednisolone 5mg since 1 year ago and I’ve been on remission since february 2017. But even not being sure if I have any problem with food, I keep my healthy diet and do yoga. I’m a pharmacist and I would prefer to be on a healthy diet that on meds but I chose to live well, and even a simple paracetamol can be dangerous! We can have side effects with any medicine, we just have to find out what is better for us. Sometimes it takes time, but I wish lucky for everyone.
Thanks for sharing, Junia. Remission is a beautiful thing.
Thank you so much for sharing your experience adding medication to your AIP lifestyle. I was also a very active, robust 35-year old when diagnosed with RA six weeks ago. I started researching options and began the AIP diet, including stoping high intensity exercise, soon thereafter. My symptoms, which were limited to my feet deemed “arthritic” by a podiatrist’s x-rays (where my journey began!) improved exponentially. Since then I’ve started to note dull aches in my wrists and hands after typing, cooking, journaling, etc. This has prompted me to revisit the idea of medication. I scheduled an intake with a rheumatologist for information gathering only and wasn’t planning to try any medications for fear of ALL that you mentioned in terms of immune suppression and side effects. After further reflection I feel differently. I don’t want to ignore what could be an unexpected yet powerful tool in my healing: conventional drugs! Your experience was informative and inspirational. I am more open to all treatment options now than I was before. It feels like a more balanced, albeit uncertain, place. Thank you!
I’m so glad, Shoshana. Wishing you complete remission, and a skilled, compassionate doctor. Thanks for writing.
I love, love, love this post. I love it because I am so happy to hear that you are doing well, but also because I can relate on such a personal level. I, too follow the Paleo approach to help control my disease activity, but it is not enough. Having read so many stories from people who have achieved remission through diet alone, I have often felt like a failure for having to take biologic medication. I wish I didn’t have to, but I had permanent damage from the onset of my RA, and I needed to act aggressively. I credit diet with helping me lower my dosages over time and I continue to view food as a medication in my rotation. Thank you for being such an inspiration. Because of you I might even try to make kombucha one day (even though the prospect scares me0. Ha!
Asa, thanks so much for writing and sharing your story. I love your description of food as a medication in your rotation. I couldn’t agree more. And in my pre-paleo days, I didn’t like kombucha at all, so I hear you! Now, I love it, though. 🙂
Great to hear it is all going well for you. I agree with you about the demonising of mainstream medicine by alternative practitioners and the way mainstream medicine demonises alternative! It’s really not helpful from a consumers point of view. I have been let down by mainstream over the years (and not just for AI issues) and tried lots of alternative treatments that either don’t work or are just impractical. And I have also been helped by both. It’s such a mine field, and your story reflects that. Thanks for sharing.
Pefectly put! Thanks for sharing your experience, Annie. Hopefully someday there won’t be such hard lines drawn between the two medical approaches.
Thank you for sharing your journey.
You’re welcome, Cathy. Sharing seems to help everyone feel less alone.
Thank you so much for this comprehensive report!
You’re so welcome, Valentina.
Eileen eloquent as ever. I greatly appreciate your honesty and openness. I have been struggling with this myself. I had unbelievable results with AIP. I don’t have a classic autoimmune disease but a genetic connective tissue disorder that acts like an autoimmune so remission is never a possibility for me so the goal is symptom control. In December I was on the road to be completely med free but then I was in a bad car accident that made me worse then I’ve been in 20 years. After 7 months of trying to manage my symptoms through diet and lifestyle, I had to finally make peace with taking medication this week. It came after I went on vacation and was miserable the whole time. I am fortunate to have wonderful doctors who have always supported my decisions and are willing to work with me to find the right treatment for me. Thank you for being inspirational.
Lisa, thank you so much for sharing your story. Having a supportive medical team is priceless, isn’t it? I’m so sorry you were miserable on your recent vacation. Hopefully the medication combined with the AIP will get you back to feeling well, so your next vacation will be joy-filled. That’s my wish for you.
Thank you for this thorough discussion of a thoughtful approach to augmenting lifestyle interventions with allopathic treatment. Bravo. If every doctor approached patients this way, I’m sure we would see better results for people with AI disease and other complex presentations.
Thanks so much, Petrolia. That is my hope for the future of medicine – that we stop drawing lines into separate camps and work cooperatively on all levels for optimal health.
Congratulations on your successes! I appreciate your transparency as you share about your journey, and I am glad you have reached this point in your journey. It is so true that each medication affects people differently. I started medication after your post a year ago and it was an encouragement as we tried different intensities. I am still balancing items, but I know supporting my body in lifestyle will ease the process. Thank you for everything you contribute to the AIP community. I love reading your posts.
Thanks so much, Elise. Wishing you success in finding that balance. Gentle hugs to you.
Eileen,
I’m so happy to hear this update! I’ve been wondering how it’s been going on your medication. I was surprised to learn of your shoulder replacement surgery but very glad to hear that you are recovering well and have a good PT. My shoulder surgery in 2014 was the tipping point for my AI condition to come on with a vengeance. I was so sick, inflamed and unprepared going in to it that I didn’t really stand a chance (in hindsight, of course ;)). As an OT, I knew that the PT I was receiving was far too aggressive but I continued for 17 weeks and ended up with another tear and severe adhesive capsulitis. A much gentler approach with neuromuscular and myofascial therapy helped tremendously! It’s all made be a more empathetic practitioner though! I look forward to hearing your surgery podcast in August! Wishing you continued health and wellness!
Blessings! Jeanne 🙂
Jeanne, I’m so sorry you had such a negative surgery and recovery experience. I’m glad you ended up with therapy that helped, and it is true that a silver lining of all struggles is that it does build empathy. You have such a positive mindset to see that. I was lucky that my PT is very balanced and non-aggressive, and my body was in excellent health pre-surgery. If I had scheduled it a year earlier when it was first suggested, I think it would have been more of a struggle for me, too. Ironically, I have an MFR appointment scheduled next week – so we think alike!
Hi Eileen- Congrats on regaining your health, vitality, and activity. ❤️ I’m one of those who kept your story in my mind all year for two reasons. 1. I greatly admire you and your work, and I was genuinely interested in your healing progress and 2. For more selfish reasons, I am trying desperately to figure out my own path.
I was diagnosed in 2014 and read the Whals Protocol the night before my first rheumatology appointment. It slowly evolved into AIP but with my aggressive RA, I needed meds early on. Methotrexate did nothing and I was on crutches for my grapefruit sized knee for eight months. Embrel and Humira gave me severe site reactions from the start. Orencia partially helped for a year, and I was able to discontinue methotrexate. Actemra made me worse. Simponi partially helped for eight months, when site reactions got too severe to continue. All the while I remained AIP, and hoped my diet and April 2017 addition of LDN would bring relief. I had a huge flare last month and decided it was time to try that Cimzia waiting in the fridge. I wish I had a rheumatologist who explained more because you taught me important things about Cimzia in this post. First- the loading dose was way too much for me, a petite woman. Two hours after my double injection, I passed out at work. Despite that, within 24 hours, 80% of my pain was gone. Honestly, I think it’s a match, probably for reasons you explained regarding targeting areas of inflammation. Unfortunately, I have not mustered the courage to take that second shot, even with skipping the loading dose, as my rheumatologist now suggests. I am hanging in there with diet, acupuncture, LDN, and an occasional aleve. However, I have high hopes for the Cimzia, should I need it. Your post has helped me stay informed and be positive about whatever choices give me my active life back. Thank you for all you do for so many.
Therese, it’s such an intense journey isn’t it? I’m not a doctor, so this is just advice from a friend, but I have 2 suggestions: If you decide to continue with Cimzia, take your Cimzia shot at night before bed, and ideally when you have the next day off if possible. That way, you can just rest through any side effects. Secondly, talk with your doctor about the timing between Cimzia shots. The goal is to get your immune system calmed down on a consistent basis so that joint damage stops happening. I don’t think it works as well if you try to take the shots on an “as needed” basis, but I could be wrong. And some people do stretch their doses out once they reach remission. So, that’s a conversation worth having with your doctor. Wishing you wellness in every way!
Thank you, Eileen. That is excellent advice, and I really appreciate it. When I returned from work after my “reaction,” I slept all day. Best to do that at night! 🙂 Keep us posted on your healing. We’ve come to know you and care about you with your wonderful blog and podcasts.
This was an incredible post for me to read right now. I was diagnosed with Hashimotos last July and in January contracted pneumonia. Although the pneumonia is gone I have been a downhill slide ever since and so far no one has the answers. I have been on a strict AIP diet since March and gluten free for 5 yrs and while a lot of crazy symptoms have subsided I am still struggling. This was a good balanced post for me to read as I am looking for a doctor to help me. I have been a natural girl all these years so going to doctors and the invasive and sometimes unhelpful things they do is overwhelming to me. Anyway thank you again for this perspective it came on a really rough day and God knew it was just what I needed to hear.
I’m so happy my sharing was helpful. Many of my friends with Hashis have found good doctors that help them find a medication that they tolerate well, which works with diet and lifestyle to help them feel their best. Wishing the same for you! Here are two other resources that might be helpful: Podcast Episode 27: Hashimotos – http://www.phoenixhelix.com/2015/09/12/episode-27-hashimotos-with-andrea-nakayama/ . And there is a patient support group on Yahoo that maintains a list of recommended doctors: https://beta.groups.yahoo.com/neo/groups/NaturalThyroidHormones/info .
Thank you I will look into both of these.
Thanks Eileen – I have really been looking forward to this post! I’m so grateful to you for all the resources you’ve pulled together here so professionally, and especially the podcast (so organised!).
So I have PsA and I just started on Humira. You might have explored this before, but any thoughts on eating certain types of food on biologics (especially fermented and unpasteurised foods)?
Holly x
You’re so welcome Cuileann. You can tell it’s a passion project for me. It’s my mission to share quality resources that can help us all.
Thank you so much for your openness and articulate description of your process. My rheumatologist isn’t sure if I have RA but wants me to try meds to see if they help joint pain and stiffness. After predisone I am on Prequenil. So far so good. Best of luck to your continued feeling better!
Thanks for your well wishes, Jenny. I’m so glad you are feeling well.
Oh, yay for you – I’m so glad – through all that trial and error – that you’ve found what works. You’ve heard the Italian girl’s name, Cinzia – pronounced ‘Chin-zia’? I kept reading ‘cimzia’ as that name, which was nice – kind of like you’d found a new friend.
Angelina, I love the symbolism! Thanks for teaching me a new friend’s name.
Really appreciate this update Eileen. Missed you at PaleoFX but said a prayer that things were working for your highest and best. We talked last year about our experiences at dinner in Austin. I’ve also gone back and forth with the meds you mention and currently taking Otezla (Ps A) & LDN… but hear you about the severe joint pain and the need to act when necessary. Hope you continue to heal fully from shoulder surgery. Sleep has continued to be so important to me lately, trumping diet. I’m cheering for you and everyone who has commented on this post and who will in the future. This is tough stuff and I wouldn’t wish it on anyone. Grateful we can support each other and share what is and isn’t working. Love to each and everyone of you. Praying for miracles. Fervently.
Hi Kristen. Yes, my dinner with you and other members of the Austin AIP community was the highlight of my trip! Thanks for sharing your experience. You are right that sleep is so essential, too.
Thank you so much for the update. Every week, when your newsletter comes, I wonder how the medication trial is going. May the stable place you’re in right now last a long time! And thanks for the positive report on shoulder replacement–>I’ll probably be having one later this year. I’ve already had both hips done (and I’m only 69), and while all 3 joints have been described as osteoarthritis, I do wonder if cartilage wear and tear is actually due to the immune system eating it away. . .p.s. I’m on methotrexate and I’ve been able to reduce the dose from 18 mg to 7.5 mg (clinical “minimum”), and the doctor is willing to consider a sub-clinical level. I’ve been pretty strict AIP for a year and a half and am just starting reintroductions. I plan to be Paleo forever.
Cecilia, thank you so much for sharing your journey. That’s wonderful that a very low dose of Mtx is effective for you. I’m going to do a podcast on surgery in August. We’ll be talking about preparing, staying paleo in the hospital, and recovery.
I was tired last night from an all-day cook-up, so I forgot 2 additional thoughts. First, I decided a few months back that a combination of AIP and medication wasn’t all bad. Second, I haven’t been on this journey too long. Your experience teaches me that something that is working today may not work tomorrow, and I need to embrace change as needed. Thank you so much for that. (And thank you for the ritual of your weekly email, with its standard structure; it’s like greeting an old friend.)
Cecilia – beautifully put!
As always, thank you for sharing, Eileen. <3
Thanks, my friend.
Thanks so much for sharing your journey with us Eileen. I can really relate to what you’ve experienced. Thank you for your courage in sharing and for all you do to inform and support those of us with RA who are really trying to thrive with this disease. Although you don’t know me I feel deeply moved by your sharing and happy to hear that you are experiencing some relief. Sending lots of love!
Thanks so much, Janet. Sending lots of love to you as well.
Oh my goodness, I had no idea about your surgery! You are amazing to have kept up your posts and podcast. Do you have to have regular lab testing for the Cimzia to monitor your mmune system? And is there a optimum dosage that worked for you? I know I have been terrified of biologics, but it is great to hear your results!
Sarah, maybe that’s why I’m suddenly tired! I did take time off for the surgery, which was definitely necessary. I was in a sling for a month, but I pre-scheduled posts and podcasts so there was no downtime for my readers and listeners. I am starting to crave a true sabbatical, though: 2-4 weeks off of work altogether. If I can’t pull it together this summer, I will definitely make it happen over the holidays. To answer your question, I get regular labwork quarterly now. They started me off with monthly and then stretched to bimonthly and now quarterly, since my labs are always good. I’m pretty tuned into my body, though, and can certainly request more bloodwork if I ever feel it’s needed. My current rheumatologist is very accommodating that way. Cimzia is typically administered as either a 200 mg injection every 2 weeks or 400 mg every 4 weeks. I do the first one – biweekly. Sometimes they start people at a higher “starter dose”, but since I had been on Humira for 6 months prior, they didn’t feel that was necessary for me, and they were right. I responded well to the normal maintenance dose.
Thank you Eileen for sharing this! I started on medication this year as well and have been waiting to hear your results. I am so happy you found something that works. I am up to 15 mg of Methotrexate and am finally seeing some results. I am hoping to be able to do some hiking on our family vacation this year. 🙂
Hiking is such a joy! That is my wish for you, too.
Hi Eileen,
Thank you for sharing your journey. You are as brave as you are beautiful! I hope your new shoulder helps you to move with grace and ease. You are my hero!
K, what a beautiful comment. You warm my heart. Thank you!
I am so happy you are doing well. I have a zero-negative inflammatory arthritis/tendonitis. I didn’t respond to methotrexate, sulfasalazine nor hydroxychloroquine even though on AIP diet. I responded within 48 hr to Humira (with low dose methotrexate). It was as if something trigger to the inflammation was suddenly turned off!! I wondered if with such a response to one dose, if I should taper the dose to response. My rheumatologist at the time said “no” take the usual dose. After 5 months, I developed severe thrombocytopenia (low platelets). So, I had to stop the biologic (which I didn’t really want to be on! but I felt very well on it). The platelets took 4-5 months to recover and as they did, the inflammation re-emerged even though I maintained an AIP diet, good sleep, etc. So, now I am on low dose prednisone (12 mg) with fantastic response as well. I am slowly tapering down while working with functional medicine to see if we can shift my inflammatory response. I just had rafts of tests done and I am waiting for results. My rheumatologist would start me on Enbrel if necessary. She also tells me that the latest European medication guidelines suggest that low dose prednisone is not as “bad” as originally considered and taking it at 0200 has the most effect with the least side-effects (because it works with our circadian rhythm). It is very clear to me that we are all individuals and although we might have similar symptoms (which lead to a diagnosis), we might in fact have slightly different mechanisms underlying the inflammation.
I love your blog, Eileen, and look forward to each edition. The recipe round-up is what I cook from! And I have learned so much from your interviews which are always so wisely done. Thank you for all the effort you put into this. I am sure you are a lifeline to many of us. Could we come up with a name for your readers….rather like Wahls’ Warriors! I can’t think of one but I’ll bet one of your readers will be very creative!
Charmaine, that’s fascinating, because my platelets plummeted on Mtx, but they ended up plateauing before it became thrombocytopenia. It looks like you and I have different responses to the same medication. It really shows that what works well for one person doesn’t always work for another. It sounds like you have a great team on your side. Is your rheumatologist or functional practitioner familiar with low-dose antibiotics? That might be worth researching, too. It’s another protocol that works for some and not for others: http://www.roadback.org/. As for coming with a special name for my Phoenix Helix Tribe, how fun would that be?! How about Rising Phoenixes?
Hi Eileen. I have actually gone down to Mark Hyman’s clinic, in Lenox MA (I live in Canada). I am waiting on receiving results of tests and starting on some supplements they have suggested. I am still on AIP with a few re-introductions (no dietary changes have made any difference but I figure gluten free is probably a healthy choice in the long run). I am hoping to uncover/correct the underlying cause for the inflammation. I appreciate too that I may need to be back on a biologic and I would go in that direction if my inflammation was out of control. I wasn’t familiar at all with the low dose antibiotics – I will do more research. Thanks for the tip.
That’s wonderful that you’re working with his clinic! I find that when people don’t respond at all to dietary changes, there usually is an underlying root cause that is driving inflammation. I hope those tests provide some clarity and effective treatment options for you, Charmaine. Wishing you wellness in every way!
Thank you for the update! I am so glad you found a medication that works for you and that your surgery went well. I love how clearly you state that the goal for you is to live the best possible life with autoimmune disease. To make that happen, we can’t think in terms of either/or or never/always.
Thanks, Jaime. Sometimes it’s a journey, getting to that realization. I think you were the first person I ever heard speak positively of medication in the paleo community. I appreciate your friendship, and your voice.
Thank you so much for sharing your experience in such detail and with such clarity. I’m glad you have found another functional tool for your toolbox!
Thanks, Quinn.
Thanks for sharing! Just one question, you write that when on MTX your ESR and CRP and other inflammatory markers were all good but you still have inflammation in your joints. Are you able to expand on this? If your bloods were good, how did you know you still had inflammation? My markers have always been within range (actually well below range) but still had pain and some joint changes but all the doctors I have been seeing in the last years have all said that the MTX was working and that I should just take painkillers for pain… not sure if this what you had also experienced and your doctors agreed to try another drug? I’m in the UK so it could be that here they don’t want to change drugs unless our blood markers are bad… thank you!
Hi Helene. It reminds me of this comic. It’s very frustrating when a doctor believes that labs trump your actual experience. The American College of Rheumatology sets standards for patient care in the USA, and they use bloodwork as part of diagnosing disease activity, but they also palpate the joints to feel for inflammation, and trust the patient’s experience of pain/disability as well. While my doctors were glad my inflammation markers had lowered (since that hopefully meant there was less stress on my organs internally), they could see very clearly that my joint inflammation remained active. If there’s any way you can find a doctor who pays attention to more than just bloodwork, you will receive better care. I don’t know how much choice you have in the UK medical system, though. Biologic medication is very expensive, so that might be part of the reason they are told not to prescribe it. https://uploads.disquscdn.com/images/40f7f1b89de1b4b4b5c709e4686c17a281c661fab1cce1a7b7f7a98b8598be5b.jpg
It’s the same with Hashi’s in the UK. If your thyroid blood markers are within the so called ‘normal’ range, your symptoms are put down to something else – depression, age, lifestyle etc..So then the doctors can prescribe more, cheap drugs.
How frustrating, Dottie! I’ve heard that this commonly happens in the US as well.