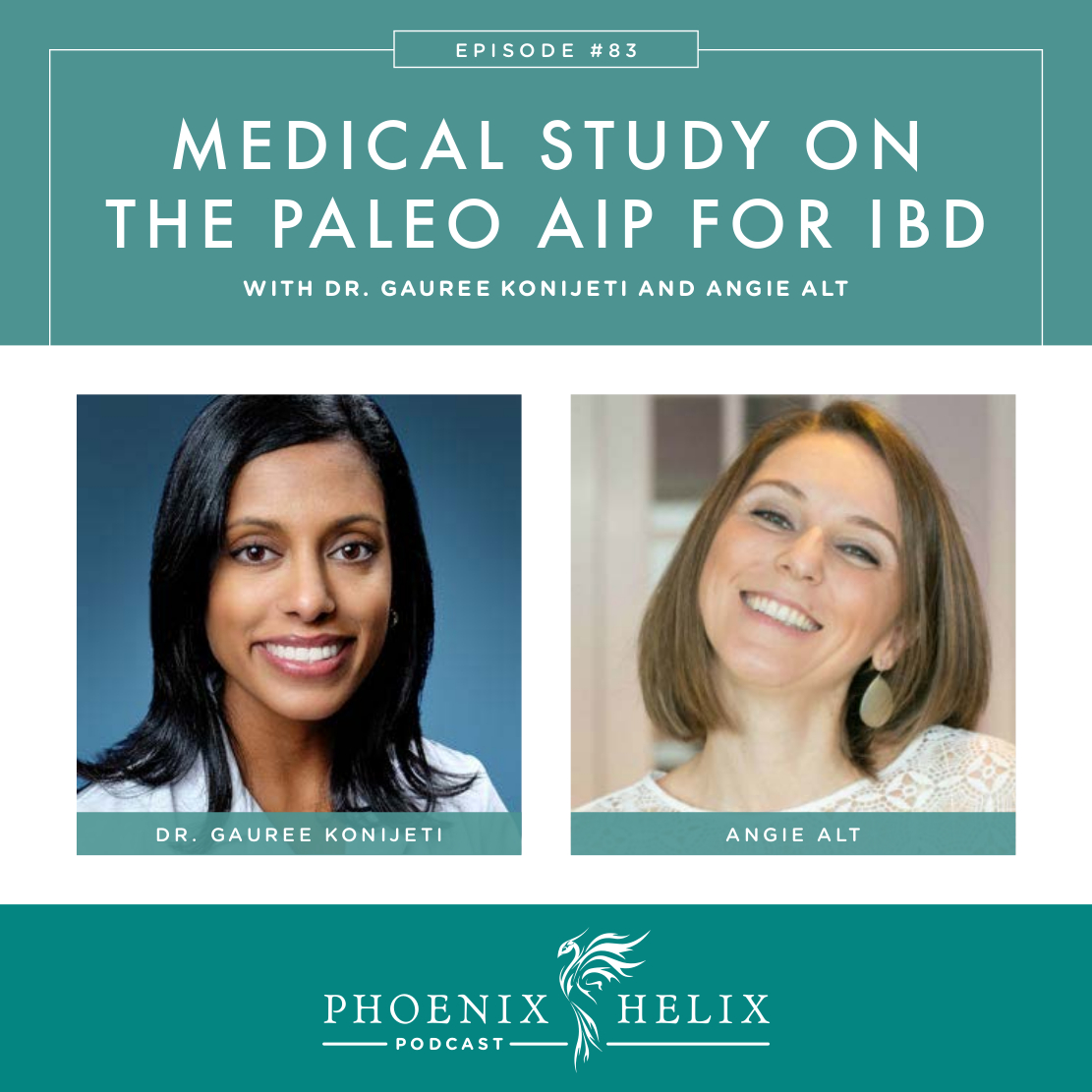
Exciting Research
There are literally thousands of anecdotal stories into the benefit of the paleo autoimmune protocol (AIP) as a treatment for autoimmune disease. But until recently, there was no scientific research to back up these claims. That changed with the publication of this study. 15 patients with active IBD (Crohn’s disease or ulcerative colitis) transitioned to the paleo autoimmune protocol. Result? 73% achieved remission. In this podcast, I interview Dr. Gauree Konijeti, gastroenterologist and lead researcher, and Angie Alt, the lead AIP coach for the group.
Listen to the Show
- Subscribe to my podcast through your favorite podcast app: iTunes, Stitcher, Google, TuneIn, Spotify, Amazon, etc.
- You can also listen to the episode right here through the player below, and if you subscribe to my newsletter you’ll get notified of future episodes.
Podcast: Play in new window | Download
Show Notes
- Intro (0:00)
- Thank You to Our Podcast Sponsor – Paleo on the Go (1:51)
- A frozen meal delivery service, they have a large menu of items for the paleo autoimmune protocol (AIP).
- Use the code PHOENIX for 10% off your first order.
- Meet Our Guests (2:53)
- Dr. Gauree Konijeti is the Director of the Inflammatory Bowel Disease Program Division of Gastroenterology at Scripps Clinic in La Jolla, California. It was a patient who introduced her to the paleo autoimmune protocol (AIP). He had severe ulcerative colitis that dramatically improved with AIP. A colonoscopy showed that his ulcers had completely healed. Dr. Konijeti has always had an interest in research. That same patient referred her to Autoimmune Wellness for more information, where she reached out to Angie Alt to collaborate on a medical study.
- Angie Alt is the author of The Alternative Autoimmune Cookbook and co-author of The Autoimmune Wellness Handbook. She has taught the AIP to over 1,500 people through her online group coaching program: SAD to AIP in SIX. She led a similar class for the group involved in this medical study. To learn more about Angie, you can listen to her personal healing story in episode 1 of this podcast.
- What is IBD? (8:15)
- IBD stands for Inflammatory Bowel Disease. It’s a category of autoimmune disease, and there are 2 types: Crohn’s disease and ulcerative colitis (UC). Ulcerative colitis is isolated to the colon and only attacks the mucosal layer. Crohn’s disease can affect the entire GI tract, and attacks multiple layers.
- The most common symptoms for both are abdominal pain, diarrhea, and rectal bleeding. Other symptoms include weight loss and vitamin deficiencies.
- The gold standard for diagnosis is a endoscopy/colonoscopy, but a complete health history and ruling out infections that can mimic IBD are important, too.
- In conventional medicine, they are often treated with similar medications. TNFa-inhibitors are systemic immunosuppressants used with many autoimmune diseases. Anti-integrins are designed to stop inflammatory cells from reaching the gut. But there are some new medications being approved for just one or the other, for differentiated treatment.
- IBS (which is often confused with IBD) stands for Irritable Bowel Syndrome, which is a collection of symptoms which can coincide with IBD but also exists outside of that diagnosis. In this study, the patients had IBD specifically. Common IBS symptoms include abdominal pain, constipation, bloating and diarrhea, but not usually bleeding. Your general physician can order a calprotectin stool test and a CRP blood test, both of which track inflammation in the body and can help differentiate between IBD and IBS.
- Medical Study Details (16:56)
- 15 patients participated: 9 with Crohn’s; 6 with UC.
- They all had active IBD, validated through endoscopy/colonoscopy. Average disease duration was 20 years.
- Most were on medication, but the drugs weren’t achieving remission. The patients continued their medication during the study, doing the AIP as a complementary treatment.
- Angie led them through a transition diet modeled after her program SAD to AIP in SIX. This was followed by a 5 week maintenance program (after they had fully transitioned to AIP).
- To measure outcomes, they did follow-up endoscopies/colonoscopies. They also tracked inflammation markers through blood and stool tests, as well as quality-of-life surveys.
- Results: 73% achieved clinical remission.
- They also gathered information related to microbiome changes and gene expression, and they’re analyzing that data now.
- Links:
- Teaching the AIP to the Study Participants (24:30)
- For the past 4 years, Angie’s been teaching an online class called SAD to AIP in SIX. It transitions people from a Standard American Diet (SAD) to the Paleo Autoimmune Protocol (AIP) over a period of 6 weeks. During that same period, nutrient-dense foods are introduced (bone broth, fermented foods, organ meat, etc.) And lifestyle changes are slowly made as well (sleep, stress management, healthy movement, etc.)
- In addition to Angie, the SAD to AIP coaching team includes 3 other health & nutrition coaches. For this study they added one additional team member: Registered Dietitian, Amy Kubal.
- They created special recommendations for anyone in the group who was currently in an IBD flare: (1) well cooked vegetables instead of raw, (2) smaller portion sizes of vegetables, (3) lean, skinless meats rather than fatty meats, (4) prioritizing soups and stews which are easy to digest, (5) choosing avocado and olive oil rather than saturated fats, and (5) avoiding coconut products. Note: These recommendations are specifically to address the diarrhea common during IBD flares; they aren’t typical AIP recommendations for everyone with autoimmune disease. As people with IBD begin to heal, they slowly transition off these recommendations.
- Resources:
- Expectations vs. Study Results (40:11)
- Angie wasn’t surprised at the 73% remission rate. After working with thousands of people, she’d seen enough success to anticipate positive results, but it was very validating to have a scientific study capture this effect.
- Dr. Konijeti was amazed by the results. She had hoped for beneficial outcomes, but didn’t expect the numbers to rival conventional drug outcomes (which they did.)
- Physician Reactions and Other Studies (42:50)
- This medical study is part of a growing body of research showing the potential benefit of dietary interventions for IBD. Her fellow gastroenterologists are very interested, but don’t know how to integrate this knowledge into their practice. Appointment times are short, resources are limited, and patients would need skilled education and support. Ideally, there would be a dietitian on staff trained in the protocol, who could then train the patients. Angie recently helped develop an AIP Certified Coach program. The book, Unconventional Medicine by Chris Kresser, provides a template for a collaborative practice model.
- Other studies on diet and IBD:
- Dr. Konijeti’s Future Research Goals (49:00)
- She’s in conversation with Scripps Clinic, where she leads their IBD program. She would like to expand to an integrative medicine model that addresses diet and lifestyle in addition to standard medical therapies. Not only does she believe this is the best way to help patients, but it would also provide the infrastructure to complete ongoing research.
- She would love to do larger studies involving more patients. She would also like to isolate factors to see which part of the AIP is the most influential in remission. And she’s also interested in whether the diet can replace medication in some cases. There are lots of avenues to explore.
- Outro (54:07)
- Dr. Gauree Konijeti is accepting new patients at Scripps Clinic in La Jolla, CA. When you call, ask for her scheduler, Natisha.
- You can keep up with Angie Alt’s work through her website Autoimmune Wellness.
- Eileen (your podcast host) is the author of multiple books, written to help people thrive with autoimmune disease. Learn more on the Books Page.
- If you like this podcast, follow or subscribe through your favorite podcast app. You can also subscribe to Eileen’s biweekly newsletter.
- Check out the entire archive of podcast episodes.
You May Also Be Interested In
Spreading the Word
If you like the podcast, please leave a positive review in iTunes. It would mean the world to me, and also helps others find the podcast. Here are some quick instructions using your iPhone:
- If you are already subscribed to my podcast: (1) Click the purple podcast icon. (2) At the bottom of the screen, click Library. (3) At the top of the screen, click Shows. (4) Click the Phoenix Helix podcast image. (5) Scroll down the page, and you’ll see Ratings and Reviews. Scroll down a little bit more and click on Write a Review. This will bring up the review screen. Tap 5 stars (if you love the podcast), and then click in the title box, and it will bring up the keyboard. Enter a title and short review. (6) Click Send in the upper right corner. (7) Thank you! Positive reviews give the podcast a higher search ranking in iTunes, helping people find it and letting them know it’s a quality podcast and worth their time to listen.
- If you haven’t subscribed to my podcast: (1) Click the purple podcast icon. (2) In the lower right corner, click the magnifying class. (3) Type Phoenix Helix in the search box. (4) Click the podcast cover in the Show list. (5) If you’d like to subscribe, click the + sign at the top of the screen. (6) To write a review, scroll down the page, and you’ll see Ratings and Reviews. Scroll down a little bit more and click on Write a Review. This will bring up the review screen. Tap 5 stars (if you love the podcast), and then click in the title box, and it will bring up the keyboard. Enter a title and short review. (7) Click Send in the upper right corner. (8) Thank you! Positive reviews give the podcast a higher search ranking in iTunes, helping people find it and letting them know it’s a quality podcast and worth their time to listen.





This is really exciting research- thanks for featuring it! It’s also great to hear a bit more about specific approaches to AiP for those with IBD. As someone with with an IBD I have kind of given up looking at AiP recipes for now, because there is so much of it that I have trouble digesting. I also just wanted to mention that I was hoping to hear someone mention Microscopic Colitis, since it seems to be an often overlooked IBD that can be incorrectly diagnosed, since there is no bleeding and biopsies need to be taken to diagnose it. Those of us who have it tend feel a bit left out of the conversation, so maybe something to consider for future shows :-). Even though it’s not “as bad” as the others, it still very debilitating.
Hi DB. I’m so glad you found the podcast helpful. I wouldn’t give up on AIP recipes; just feel free to adapt them as necessary to your needs. All of us personalize the diet to some extent. I was also really happy that Angie shared the details on how they adapted it for this study. Thanks also for sharing your diagnosis and experience. Dr. Konijeti did say that diagnosis is an art, and I think most great doctors agree. I think it was helpful that she mentioned the blood tests that can show inflammation when symptoms aren’t clear. We are a diverse tribe, and you are very much a part of it. Wishing you wellness in every way.
I’m so thrilled that you did these interviews…thank you one again for being THE best interviewer at presenting relevant and credible information. Gives me some hope! Through my own experience (I did strict AIP for 6 months with no change) I know that AIP requires some tweaks for those of us with IBD. I understand that even within the modifications for IBDers each person was further counselled by a dietician. I’m commenting here with the hope that someone with knowledge might reply. It would be so great to see a menu template because I’m curious what filled up the missing calories/volume in the short term while the participants guts were ‘healing’. More lean protein / more olive oil? I also wonder what the favoured probiotic sources were.
Hi Heidi. I think you answered your own question in terms of filling in calories. The goal is always to focus on what we can eat rather than what we can’t. In terms of your other question, probiotics aren’t required on the AIP and they weren’t mentioned during the interview, so I don’t believe they were part of this medical study. (I read the full study text and there was no mention of probiotics.) Instead, as Angie said, fermented foods were recommended, which is part of the AIP. Sauerkraut is a great choice. Here’s my favorite recipe: http://www.phoenixhelix.com/2013/05/08/no-fail-no-pound-sauerkraut/ . If you would like individual dietary counseling, Amy Kubal (the dietitian on this study) works through Robb Wolf’s website, and you can schedule a consult with her over Skype: https://robbwolf.com/about/